University of Auckland researchers are developing a medical device to help assess hearing loss and deliver compounds and other treatments.
Hearing loss caused by damage to the inner ear(sensorineural hearing loss) – the most common kind – is a challenge to diagnose and treat. University of Auckland researchers Professor Peter Thorne and Dr Haruna Suzuki-Kerr are on a mission to change that – with the help of a sheep’s skull and technology.
Hearing loss affects almost one in six New Zealanders – that’s around 880,000 people – and this is expected to rise as our population ages. “Sensorineural hearing loss happens gradually. It varies widely across individuals. We have no way to stop it, and it’s irreversible. We have hearing aids and cochlear implants, but we’re missing a drug-based option,” says Suzuki-Kerr, who is an auditory physiologist.
“Hearing tests tell you whether hearing is working or not working but nothing more than that. The damaged cells in the inner ear are so far inside the skull beyond the ear canal. It’s hard to understand what’s happening, why cells are damaged or dying,” says Thorne, who specialises in auditory neuroscience.
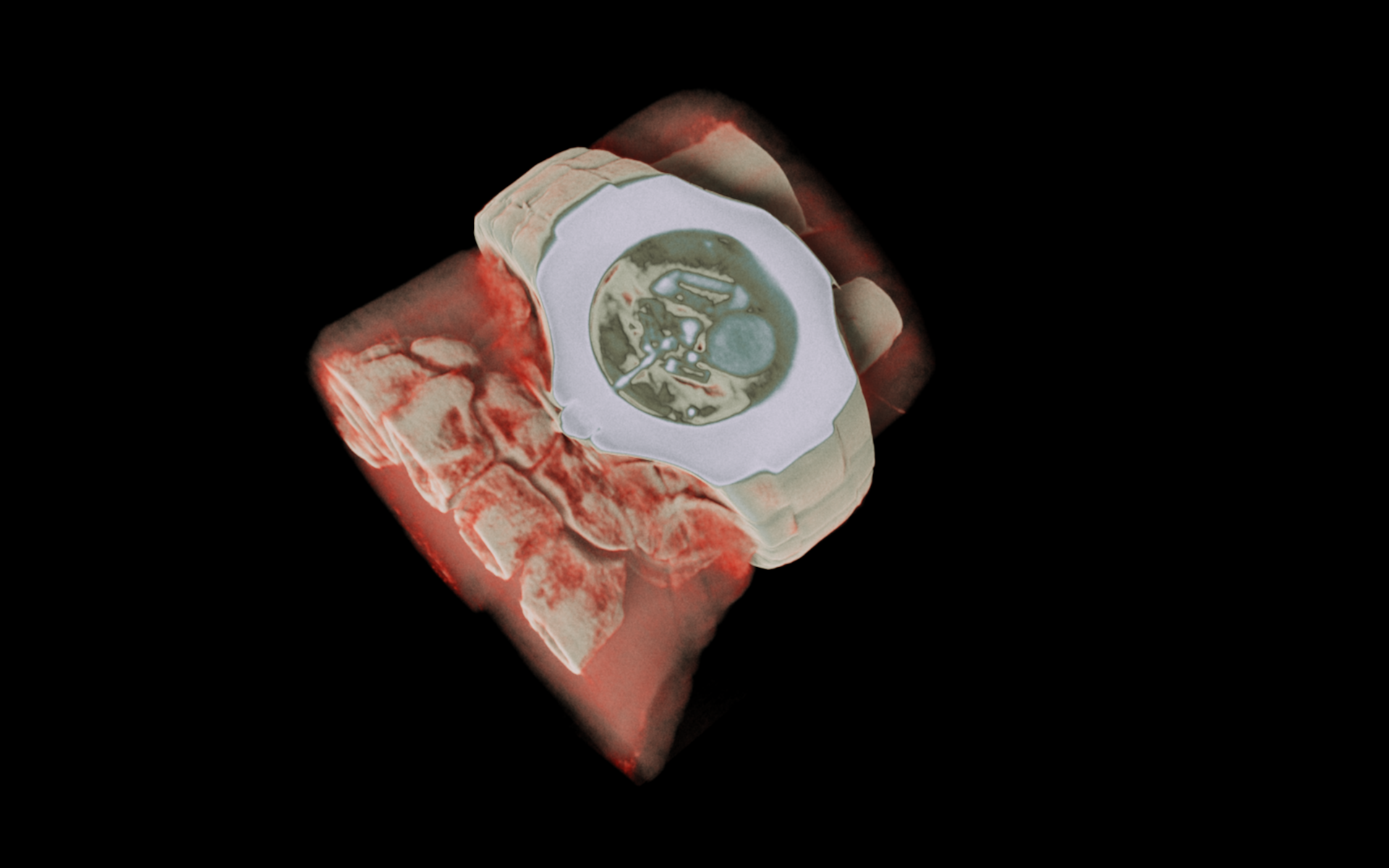
Their goal is a medical device that can be inserted down the ear canal and through a small hole in the eardrum to assess the cochlea, and quickly deliver compounds and other treatments. Achieving this will require Thorne and Suzuki-Kerr and their team to solve three key questions: How to identify what’s going on inside the cochlea, how to get therapies into the cochlea, and how to reach all parts of the cochlea.
The structure of the ear also presents challenges. The ear canal is like a tunnel with twists and turns on the way to the cochlea, with a ‘window’ covered in a clear membrane separating the middle and inner ear.
“We believe the solution lies with a new type of medical device, one that can measure what’s going in the inner ear, from the composition of the fluid through to pushing compounds through the membrane and into the cochlear,” says Thorne.
In 2024, Thorne and his team secured five years of research funding from MBIE’s Endeavour Fund to continue their work.
“We now have a prototype device to efficiently deliver drugs into the cochlea via the ear canal. We’ve produced pilot data using optical tools to investigate and assess the cochlea and its fluids,” says Thorne.
This is where the sheep model comes in. Suzuki-Kerry says the anatomy of a sheep’s ears is very similar to human ears, making them a good model for testing their device. Thorne says the work they’ve done using the sheep’s skull is a world-leading programme.
The concept began back in2018, with experts from the then-MedTech Centre of Research Excellence, Brain Research New Zealand, and across the University’s medical, science and engineering faculties.
“We were taking big ideas into the research and clinical communities with the goal of the best getting the funding. The idea of getting compounds into the inner ear came from one of those meetings. From there, we got help from Callaghan Innovation, and funding from the MBIE Smart Ideas fun and Te Tītoki Mataora research translator.
“Seed fundings enabled us to develop our capabilities and research plan towards a larger funding, and create a remarkable group of scientists and clinicians, supported by Iwi United Engaged on collaborative community engagement,” says Thorne. Suzuki-Kerr says, “having a community of people to both support and collaborate with us has been a highlight of our work so far.”
“Many of the original team are still with us and continue to be a part of our journey, but as we’ve developed we’ve added other skills and experience,” says Thorne.
Their goal is to establish a New Zealand-based company to manufacture the device, creating a new industry for inner ear therapeutics, and added economic benefit to New Zealand through global investment and pharmaceutical company collaborations.
“Māori are disproportionately impacted by hearing loss and less likely to access treatment. Poorly managed hearing loss has considerable impact on children and adults and costs New Zealand around $4.6 billion annually. We need alternative forms of treatment to hearing aids or cochlear implants to reduce the burden of hearing loss,” says Thorne.
He says if successful, their programme could transform the treatment of hearing loss to enable rapid assessment and precision treatment that will be more broadly accessible and cost-effective than current treatments.
.jpg)
.jpg)