Our perception of pressure is subjective. We can’t quantify the pressure we apply to objects around us, nor to our own bodies.
Research fellow Dr Massi Hesam, from the Auckland Bioengineering Institute is working on a new approach using her bioengineering skills.
“First, we need to understand more about pressure. Have you ever had a friend give you a handshake that’s way too strong? Chances are you’re aware of it but your friend isn’t. Skin doesn’t measure pressure; rather, we perceive pressure subjectively. So, we need to know how much pressure to apply."
“For some medical treatments - such as compression therapy for lymphedema, chiropractic care, and physiotherapy - massage or compression techniques do not provide any measurable data to clinicians. As a result, there is often a degree of guesswork involved. Reliable data from compression at the body interface can overcome the limitations of subjective human pressure perception, provided there is also a method to interpret that data. This would enable treatment to be personalised, from baseline assessments through to ongoing therapy sessions,” says Hesam.
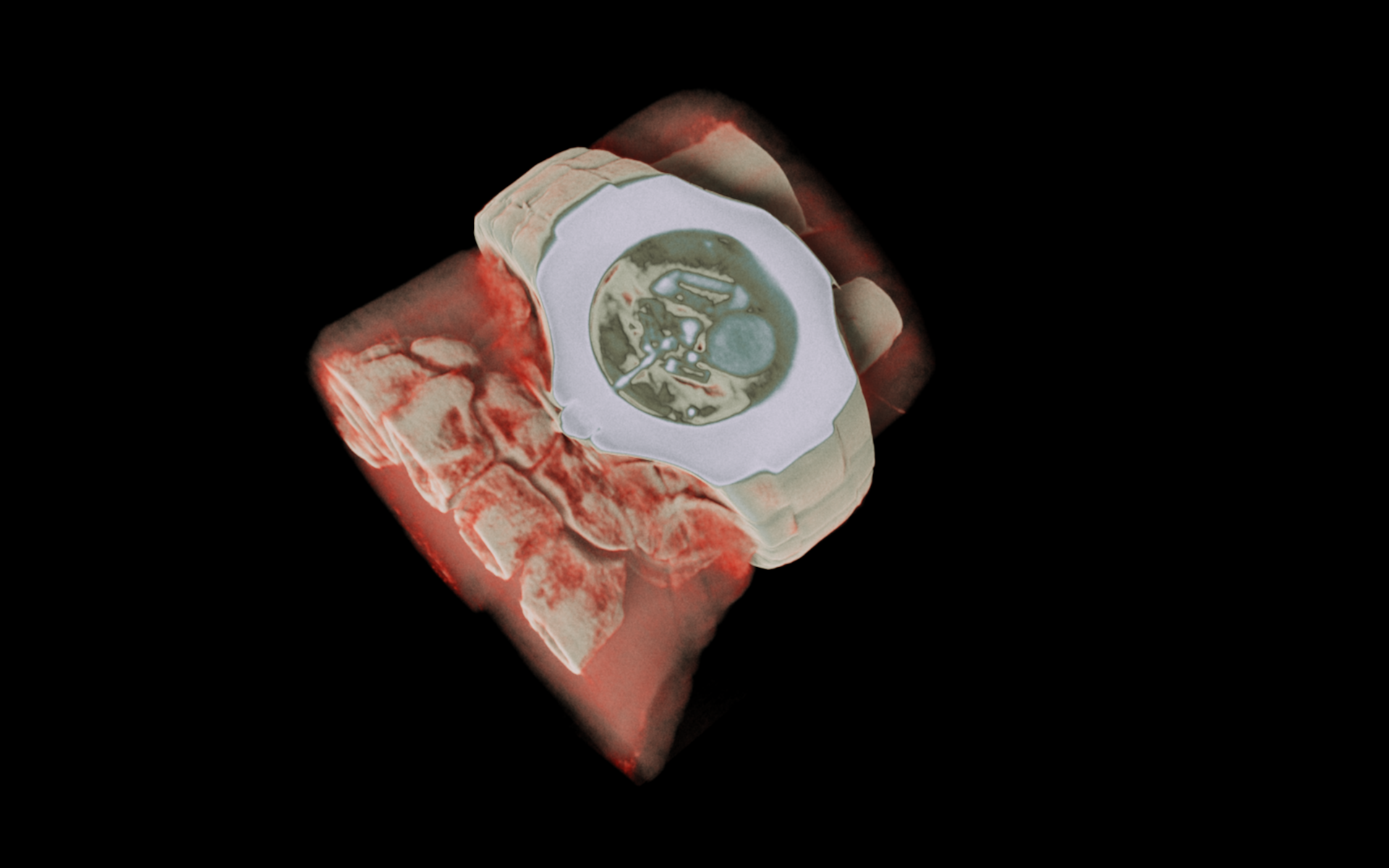
“I am developing a monitoring system for improve the efficacy of Intermittent Pneumatic Compression, or IPC treatment. IPC is a therapy that uses inflatable sleeves or garments to gently squeeze parts of the body, usually the legs or arms. This helps improve blood flow and reduce swelling by mimicking the natural muscle movements that push fluid through the body. It’s often used for people with poor circulation or conditions like lymphedema.,” says Hesam.
“IPC is already available but I want to improve the efficacy of the treatment by adding a monitoring system to it. Currently, IPC treatment is set up based on subjective patient feedback and visual observation by clinicians. Our technology offers real-time measurement of the pressure applied by the IPC suit to the patient’s body, enabling clinicians to adjust the treatment setup more accurately.”
Her solution is real-time measurement of the pressure applied by the IPC suit on the patient’s body, enabling clinicians to adjust the treatment setup more accurately. Hesam and her team are developing a smart garment that covers affected areas of the body and is equipped with numerous pressure sensors.
“The patient wears our smart garment over the area affected by oedema and the IPC suit is wrapped over the smart garment. Clinicians adjust the treatment setup based on the real-time pressure data provided by the garment.”
From here, they plan to automate the treatment setup by training an AI algorithm to customise the pressure according to each patient's needs. “Our current version of the garment includes only compression sensors to measure pressure at the body interface, but we are now working on integrating Bioelectrical Impedance Spectroscopy (BIS) sensors to monitor oedema volume in real-time. This will help train the AI model more accurately. After each treatment in the suit, the clinician will also receive data to help plan future treatments,” says Hesam.
A key application for this personalised IPC treatment will be patients with lymphoedema which can be an unpleasant side-effect after cancer treatment, particularly for women with breast cancer who have had lymph nodes removed. Lymphatic fluid builds up, mostly in the arms or legs, because the drainage system isn’t working properly. Globally, around 250 million people re affected like this, with their quality of life significantly affected and an accompanying burden on the healthcare system.
She is already seeing other potential uses for the smart garment. “It could be used for monitoring pressure at the body interface for hospitalised patients who must remain in bed for extended periods and are at risk of developing bedsores. Current smart mattresses can help, but they only provide feedback from body regions in direct contact with the mattress. Our garment can provide data from areas under pressure that are not directly touching the mattress.
“Our sensing technology could also be used in the training of chiropractors and physiotherapists to help them adjust their hand pressure during treatment procedures.”
Hesam developed her proof of concept earlier in 2025, ensuring the proposed “suit” could measure a range of pressures through its sensors, and that it was unisex. The prototype suit is now being tested in New Zealand clinical environment to demonstrate how it works, how it provides feedback to end-users, and the value of the AI-driven data it produces.
Hesam is focused on commercialisation and is already working with US-based Medella Health and their Flowpresso® lymphatic drainage technology on that journey.

.jpg)