Ella Guy was researching algorithms for modelling respiratory function for control of mechanical ventilation when doctors told her they had limited lung function data available from patients in between hospital visits.
“So, there went my PhD,” says Guy as without frequent data, control is limited. To increase available data we “needed a way to test over time, and a device to make this happen”. Ella started out more interested in computational modelling, having done mechanical engineering as her undergraduate degree, but this changed her direction.
“You could describe my new pathway as happening in a series of happy accidents, a lot of good advisors who helped shape what I was doing, and the conclusion that I had no choice but to solve the problem.”
Chronic respiratory disease (CRD) is our third biggest killer, but a new tool developed by Guy and supervisors Dr Lui Holder-Pearson and Dist. Prof.Chase at Te Whare Wānanga o Waitaha University of Canterbury (UC) could well change the way we manage it.
Guy wrote her thesis on how we might go about changing the way we approach respiratory diagnostics and monitoring, from novel low-cost hardware to advanced digital twin models, focusing on combining new algorithms with more comprehensive and accessible monitoring.
Our CRD problem is growing, according to a 2023 report by the Asthma and Respiratory Foundation NZ. Respiratory disease affects more than a million New Zealanders – that’s one in five of us. Care costs NZ$8 billion a year, and causes one in 11 hospital stays. That’s 82,500 admissions of whom a third are children – 26,300 in total. CRD is our third leading cause of death. Prevalence of these illnesses is increasing, particularly for conditions like asthma, COPD, and bronchiectasis, with a significant impact on hospitalisations and a strong link to socioeconomic deprivation, especially in areas with high Māori and Pacific populations. Globally,the burden is increasing, directly affecting approximately 450 million people. During the time it took Guy to complete her PhD, New Zealand’s rate of CRD rose from one in seven to one in five people.
“Measuring CRD variables is difficult and often impractical, with significant added economic and social costs. We need a new approach to establish patient-specific baseline functions and track progression of lung function and mechanics over time, without requiring clinical visits and multiple intrusive tests for each data point,” says Guy.
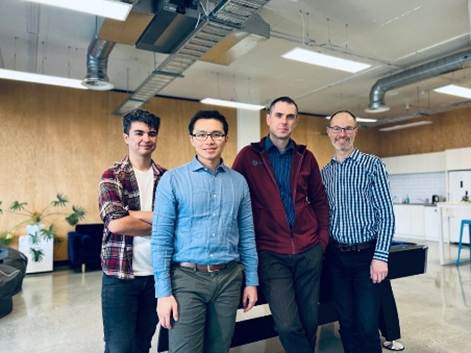
A team at the University of Canterbury (Guy, Lui Holder-Pearson, Geoff Chase, and PhD students Jaimey Clifton, Trudy Caljé-van der Klei, Sam Hastings, Kirsty Hawke and Jordan Hill) now works to develop and optimise the device and software for multiple respiratory disease applications. The device – BOB, or Breath-to-Breath Observed Biometrics – is a simple solution providing real-time, high quality, breath-to-breath data, for the patient and their clinician to use. The team is also partnering with clinical, social science, cultural, and commercial teams and advisors to ensure that solutions are developed to meet patient and clinical needs.
“Current testing for respiratory illnesses can be both lengthy and costly. A diagnosis can take multiple visits to specialised clinics, but not everyone can access such facilities. Current testing can be hard to access outside main centres, have long waits for appointments, and be difficult for children, elderly and those with severe illnesses.
“With BOB, more frequent monitoring can be as simple as breathing normally into the device each morning. This improved monitoring should help reduce pressures on scarce healthcare resources, and provide daily tracking to ensure the patient is receiving optimal care. We’ve created specialized digital twin models and software to interpret and send these results to the patient’s GP, providing data-driven care that isn’t currently possible with in-appointment testing,” says Guy.
BOB can also be used in conjunction with Continuous Positive Airway Pressure (CPAP) devices used to treat sleep apnea and COPD, to optimise how that device is used.
Guy aims to have a prototype BOB suitable for regular clinical use ready in February 2026 along with more baseline data from healthy patients to help to assess clinical feasibility. “I learnt from my RAP-funded work that patients and clinicians need actionable data for this to become part of a valid care plan.”
Down the track Guy believes BOB could develop into a home-based monitoring system, similar to the CEG approach for diabetes, increasing patient knowledge and control of their condition.
“My main interest is health literacy. BOB might help address inequities around access to monitoring and care. Patients with limited access to specialist care because of distance means data collection is infrequent, often providing only a snapshot rather than enough data to enable evaluate and make decisions about long-term care.”
While Guy’s goal is commercialisation, the next 12 months will see her focusing on more longitudinal testing, making BOB usable for both clinicians and patients, establishing whether they can track with accuracy over time, and looking at equity issues.